
- Centro Médico TeknonCentre Mèdic Quirónsalud Badalona
 Why do you have burning?
Why do you have burning?
Although there is a large amount of acid (hydrochloric acid) in the stomach, it is normal that they do not cause discomfort because their walls are prepared to withstand it. However, when acid rises from the stomach into the esophagus you have the burning sensation (and sometimes pain) because the walls of the esophagus are more sensitive. Therefore, in most cases, burning is due to the passage of acid from the stomach into the esophagus. This is called "gastroesophageal reflux" ("reflux" of backward flow and "gastroesophageal" indicating the direction from stomach (gastro) to esophagus.
Why are burns sometimes held in "the pit of the stomach" and other times they go up the chest?
The location of the burning sensation depends on whether the acid rises more or less up the esophagus: if it rises little the burning can be noticed in what is vulgarly called "the mouth of the stomach", which actually corresponds to the union of the esophagus with the stomach; If the acid rises higher, the burning sensation can even reach the neck.
Why does gastroesophageal reflux occur?
Normally, the acid is in the stomach and does not rise into the esophagus. For this there is a valve (cardia) that allows food to pass from the esophagus to the stomach but prevents the acid, and the food itself, from receding (refluxing). On certain occasions this valve fails (its strength decreases) and then gastroesophageal reflux occurs.
Is hiatal hernia the same as gastroesophageal reflux?
It is not the same, although sometimes they can coincide. In addition, many doctors say that a patient has hiatal hernia when, in reality, he has acid reflux from the stomach into the esophagus. A hiatal hernia is actually a part of the stomach moving up (slipping) from the abdomen to the chest. Many people have hiatal hernia and no reflux, although it can help it.
Is it normal to have burning?
Having burning is not normal, although we can all have them at some time, especially if we have eaten or drunk excessively or after certain strong meals. The importance of burning depends on whether they appear frequently or are intense. The frequent presence of burning should be a reason for the patient to go to the doctor, not because it is something dangerous but because there are excellent treatments to avoid them. At other times, gastroesophageal reflux may produce other symptoms. Among them is regurgitation ("returns to the mouth") of already swallowed food or stomach liquid. Difficulty swallowing, chest pain, throat irritation, and even coughing can be caused by the reflux of acid from the stomach into the esophagus.
Do I need to have tests to diagnose this disease?
In most cases the doctor can make the diagnosis of gastroesophageal reflux just knowing the patient's discomfort. However, on certain occasions it is necessary to visualize the esophagus inside to see if there is inflammation and know its intensity. This is because there is no good correlation between the symptoms reported by the patient and the degree of damage produced in the esophagus. The best test for this goal is endoscopy (direct viewing of the esophagus through a probe inserted by mouth). More rarely it is necessary to measure the amount of acid that refluxes; for this, a very thin probe is used that is inserted through the nose (pH 24h)
What are the things that favor the ardours?
Gastroesophageal reflux, and therefore burning, are favored by various circumstances. It is more common to occur when lying down or when one leans forward. It is also related to certain foods and drinks such as chocolate, coffee, mint, alcohol or fatty foods. Certain medications can also promote reflux. Finally, it is normal for burning to occur during pregnancy.
What is the treatment of gastroesophageal reflux?
The type of treatment will depend on the intensity and frequency of discomfort. If they appear sporadically, it will be sufficient to take antacids when burning appears (eg Almax, Gelodrox, Bemolan, etc.). When the symptoms are more frequent it is preferable to reduce the amount of acid that is produced in the stomach. For this there are many drugs, some less potent (eg ranitidine, famotidine) and others more potent (eg omeprazole, lansoprazole, pantoprazole). They are generally effective and have hardly any adverse effects.
How long should the medication be taken?
The problem with gastroesophageal reflux is that, in many cases, it is chronic; That is, when you stop taking the medication the symptoms reappear. Therefore, a large number of patients have to do the treatment for a long time, even for a lifetime.
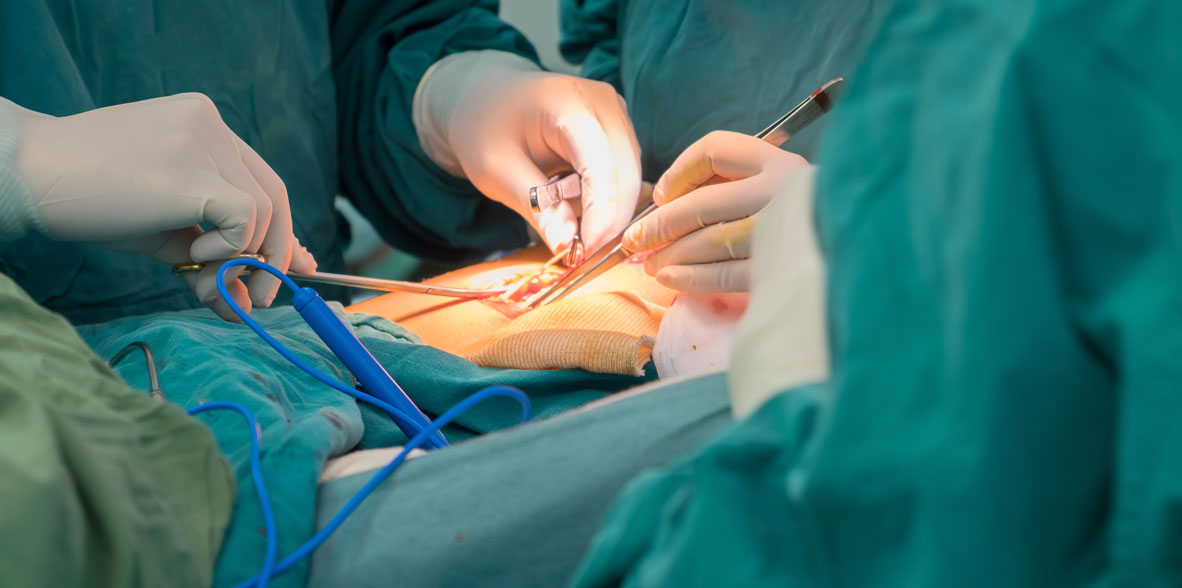
Is this disease operated?
Yes, gastroesophageal reflux can be operated. Surgery is usually done in severe cases, or when patients do not want to take medicine for a long time.
Surgical treatment aims to reconstruct an anti-reflux barrier. The most widely accepted surgical technique is fundoplication, which involves bolstering the function of the cardia by wrapping the upper part of the stomach around the lower portion of the esophagus. The approach to surgical intervention is in principle by laparoscopy. Currently, the indications for surgery are medication failure (frequent recurrences, intolerance to pharmacological treatment) and/or the express wish of the patient.
It is accepted that fundoplication obtains the best results in the long term, and therefore it is the preferred technique. Total and partial fundoplications, in uncontrolled trials, obtain positive results, with a success rate close to 90% at 10 years, in the control of GERD symptoms, acid exposure and absence of endoscopic lesions.
Although there is not enough information about the long-term benefits of surgical compared to medical treatment in patients with esophagitis, preliminary data point towards similar effectiveness. A randomized trial in patients with GERD and esophagitis compared long-term medical treatment with PPIs (omeprazole) versus conventional anti-reflux surgery. The 3-year and 5-year outcomes showed slightly higher effectiveness and favorable impact on quality of life for surgery, but similar if the dose of omeprazole was adjusted to 40-60 mg/day. Recently, a study has provided long-term results (12 years), concluding that both prevent stenosis and adenocarcinoma of the esophagus in a similar way. A large portion of the patients in this study, all with severe GERD, continued to need medical treatment 10 years later (62% of those undergoing surgical treatment and 92% of those in the medical treatment group).
Operative mortality is generally less than 0.5%, and is not related to the type of intervention performed. The risk of undergoing this type of surgery is greater than that of developing esophageal adenocarcinoma, even in the high-risk population.
The overall morbidity of groups with extensive experience in this type of intervention is close to 5%, including medical and surgical complications, and the symptoms reported by patients after surgical correction are scarce, but of various kinds (dysphagia, inability to burp (gas-bloat syndrome), inability to vomit, postprandial fullness, early satiety, abdominal or chest pain and aerophagia or increased meteorism). Anti-reflux surgery is a therapeutic alternative comparable in effectiveness to the pharmacological treatment of patients with GERD, with the advantage of solving the problem definitively and avoiding the patient having to take medication all his life.
It is necessary to personalize the option of surgical treatment and inform the patient of its existence and its benefits and risks. In general, the context, the experience of the surgical team and the patient's preferences play a very important role