
Achalasia of the esophagus is a rare disease characterized by poor esophageal clearance. Esophageal evacuation is limited due to poor esophageal peristalsis, a lack of relaxation of the lower esophagus sphincter after swallowing and in a small group of patients, this is aggravated by the presence of a lower esophagus sphincter with high pressure.
The alteration of the esophageal emptying leads to a progressive dilation of the esophagus.
Diagnosis and Symptoms
The two symptoms most commonly present in patients with achalasia are dysphagia and regurgitation. Dysphagia is one of the first symptoms to manifest and is caused by the lack of relaxation of the lower esophagus sphincter (LES). As the esophagus progressively dilates and begins to accumulate food inside, regurgitation occurs.
Nocturnal regurgitation can cause aspiration pneumonia and lung abscesses. This disease is of slow evolution so the symptoms of esophageal malevacuation appear only after several years. In more than half of patients, dysphagia leads to weight loss.
For diagnosis, manometry, endoscopy and radiology are needed. Manometry is the study of choice when achalasia is suspected. Typical findings include: absence of esophageal peristalsis, inadequate relaxation (impossibility of complete relaxation), and increased LES tone.
Digestive endoscopy should be performed in all patients to rule out the presence of other common causes of dysphagia such as Schatzki's ring and benign or malignant narrowings. The finding of a dilated esophagus with a narrow LES is characteristic of Achalasia.
By carefully advancing the endoscope, it can easily pass through the LES into the stomach. This is not observed when faced with the presence of a narrowness of malignant origin where the rigidity of the tumor prevents the advancement of the endoscope into the stomach.
The study contrasted with barium shows the typical findings: the mouse tail in the distal part of the esophagus and a dilated esophagus in the proximal part of it. A hydroaerean level behind the heart may be seen on plain chest x-ray. Endoscopic ultrasound is useful to demonstrate the presence of a hypertrophic muscle layer of muscle.
Treatment
The treatment is aimed at decreasing the resistance of the passage through the cardia. This can be achieved through the use of medications, balloon dilations or surgery. Calcium blockers or nitrite-based medications are ineffective in most patients.
Recent experiences with endoscopic injections with botulinum toxin into the wall of the distal esophagus (LES) suggest that symptoms may be alleviated in 2/3 of patients, particularly in the elderly.
Unfortunately the effect is temporary and although when the initial injection improves the symptoms the effect does not last more than 3 to 9 months.
Balloon dilation of the esophagus is effective in more than 2/3 of patients but usually requires multiple sessions that may be accompanied by complications (perforation). However, when dysphagia improves, more than half of patients develop gastroesophageal reflux. Like Botulinum Toxin, the effect of dilation is temporary with a recurrence of between 2 to 5 years.
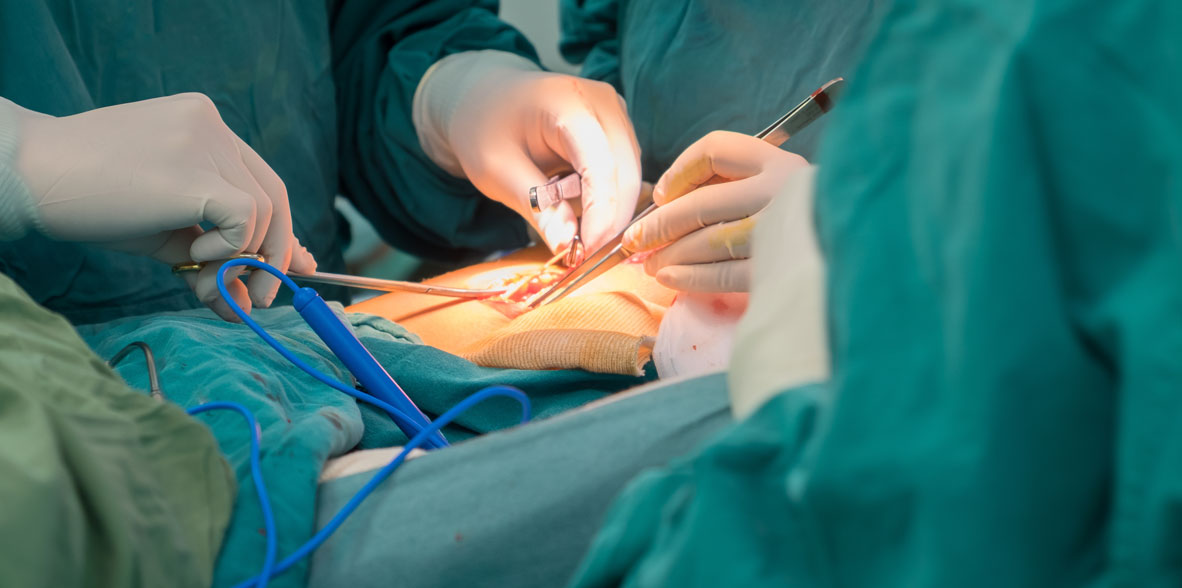
Esophageal myotomy should be considered in patients without surgical risk. The procedure is performed openly (laparotomic or thoracic) or minimally invasive (laparoscopic or thoracoscopic). A 5 to 6 cm myotomy that crosses the gastroesophageal junction and divides the muscularis of the lower esophagus and upper stomach is effective in relieving dysphagia in 95% of patients. If the procedure is performed from the abdomen, a partial fundoplication may be added to prevent reflux. This procedure has the benefit of restoring the ability to swallow without adding the problems of reflux.
Risks
In those patients in whom elective esophageal myotomy is performed, mortality is less than 0.3%. The risk of recurrence of dysphagia in patients presenting with classic manometric findings is approximately 5-10%. In patients with atypical findings (e.g., vigorous achalasia), the risk of recurrence is higher.
The main intraoperative complication is mucosal laceration. The laceration is usually easily recognized and can be repaired with sutures. Major complications in patients where no procedure is performed are progressive malnutrition and aspiration pneumonia. If the chosen route is endoscopy (laparoscopy or thoracoscopy), the conversion to the open route in case of difficulties in identifying the anatomy should not be taken as a complication, but on the contrary, as a wise decision to be able to perform the surgery safely.
Results
After esophageal myotomy, 90% of patients have good long-term outcomes. Reflux is rare if any anti-reflux procedure was added. Otherwise, reflux is seen in about 50% of patients. In most patients at low surgical risk (ASA I and II) esophageal myotomy requires 1 to 3 days of admission. Older or high-risk patients (ASA 3 and 4) may need longer hospitalization. After an uncomplicated myotomy, patients can begin drinking fluids the same night of surgery or as soon as they recover from the effects of pneumoperitoneum (mainly nausea). A solid diet is usually tolerated within 1 or 2 days. Patients should have a semi-solid diet for about 4 to 5 weeks.



































