
- Centro Médico TeknonCentre Mèdic Quirónsalud Badalona
What is esophageal cancer?
The esophagus is a muscular duct that connects the throat to the stomach and allows food to enter the stomach to be digested. Usually, the esophagus is between 25 and 35 centimeters long (10 to 13 inches). The normal width of an adult person's esophagus is about 19 millimeters (about 3/4 inch) at the narrowest point. The wall of the esophagus has several layers. Because cancer of the esophagus begins in the inner layer and grows outward, these normal layers can be used as landmarks to describe the progression of the tumor. The innermost layer of the esophagus is called the mucosa.
The mucosa consists of two parts. The epithelium constitutes the very layer of the esophagus. The flat, thin cells of the epithelium are called squamous cells. The lamina propria is a thin layer of connective tissue located beneath the epithelium. Under the mucosa is a thin layer of muscle tissue called muscularis mucosae. The next layer is the submucosa. Some parts of the esophagus have glands that secrete mucus into this layer. The layer below the submucosa is a thick band of muscle called muscularis propria.
This muscle layer contracts rhythmically and in coordination to push food along the esophagus from the throat to the stomach.
The outermost layer of the esophagus is made up of connective tissue and is called adventitia.
The upper part of the esophagus has at its beginning a special muscular area that relaxes to open the esophagus when it feels that a food or liquid is approaching. This muscle is called the upper esophageal sphincter. The lower part of the esophagus is connected to the stomach. This connection is called the gastroesophageal junction or GE junction. Near the GE junction is a special muscular area called the lower esophageal sphincter, which not only controls the outflow of food from the esophagus into the stomach, but also prevents acid and digestive enzymes found in the stomach from passing into the esophagus. The stomach contains strong acid and enzymes that digest food. The epithelium or lining of the stomach is made up of glandular cells that release acid, enzymes and mucus.
These cells have special characteristics that protect them from acid and digestive enzymes found in the stomach.
If acid passes from the stomach into the esophagus, patients may feel a burning sensation in the middle of the chest called heartburn (acedia). The medical term used to refer to the passage of stomach acid into the esophagus is reflux. If the reflux of stomach acid into the lower esophagus is prolonged for a long time, this acid can cause the squamous cells that usually cover the esophagus to be replaced by glandular-type cells. These glandular cells usually resemble the cells lining the stomach, and are more resistant to gastric acid. If these glandular cells extend more than 3 centimeters (about 1 1/4 inches) above the junction of the esophagus and stomach (GE junction), the patient has a condition called Barrett's esophagus. These new glandular cells that make up Barrett's esophagus may later become precancerous. These cells can develop into cancer, so it's important for people with Barrett's esophagus to be taken care of.Dare observation.
There are two main types of esophageal cancer. One of them is called squamous cell carcinoma. This name comes from the type of cell that becomes cancerous. In the past, this type of esophageal cancer was the more common of the two types, accounting for nearly 90% of all cases. However, more recent medical studies show that, at present, squamous cell cancer only accounts for about 50% of esophageal cancer cases. Because the entire esophagus is usually covered with these types of cells, squamous cell carcinoma can occur anywhere along the esophagus.
The other common type of cancer of the esophagus is called adenocarcinoma. This type of cancer begins in glandular tissue that does not normally cover the esophagus. Before adenocarcinoma can develop, an area of squamous cell must be replaced by glandular cells, as in the case of Barrett's esophagus.
What are the main statistics about esophageal cancer?
The American Cancer Society estimates that approximately 2003,13 new cases of esophageal cancer will be diagnosed in the United States in 900 (10,600 men and 3,300 women). These figures include all groups of the general U.S. population, including Hispanics.
This disease is about three times more common among men than women, and almost three times more common among blacks than among whites. Squamous cell carcinoma is the most common type of esophageal cancer among blacks, while adenocarcinoma is more common in whites.
Esophageal cancer is much more common in other countries. For example, esophageal cancer rates in Iran, northern China, India, and southern Africa are 10 to 100 times higher than in the United States.
The American Cancer Society estimates that 2003,13 deaths from esophageal cancer (000,9 men and 900,3 women) will occur during 100. Most people with esophageal cancer will eventually die from this disease, as it is usually diagnosed at an advanced stage. However, survival rates have been improving. In the early 60s, only 4% of all white patients and 1% of all black patients survived 5 years after diagnosis. Currently, 13% of all white patients and 9% of all black patients have survived 5 years after diagnosis.
The 5-year survival rate refers to the percentage of patients who live at least 5 years after they are diagnosed with cancer. Many of these patients live much longer than 5 years after diagnosis. 5-year survival rates are used to produce a conventional way of discussing prognosis. The five-year relative survival rate excludes from the estimates patients who have died due to other diseases, and is considered to be a more accurate way to describe the prognosis of patients with a particular type and stage of cancer. Of course, 5-year rates are based on patients diagnosed and initially treated more than five years ago. Improved treatments often result in a more favorable prognosis for newly diagnosed patients.
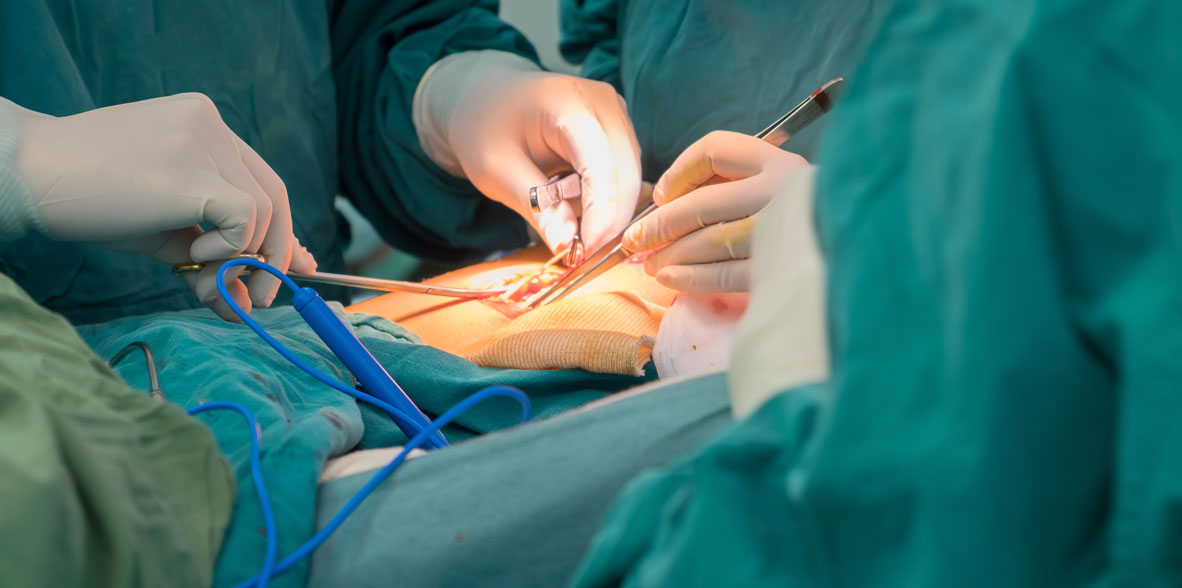
Surgical treatment of esophageal cancer
Esophageal carcinoma is a relatively rare but highly lethal condition, accounting for 5% of gastrointestinal tumors in the United States.
An estimated 12,300 patients developed esophageal carcinoma in the United States in 2000. In most Western countries the prevalence of esophageal carcinoma is increasing at approximately 10% per year, faster than any other malignant tumor.
This disease has undergone a profound epidemiological change, from the prevalence of squamous cell carcinoma associated with tobacco and alcohol abuse, to adenocarcinoma associated with gastroesophageal reflux (GER) and metaplasia of Barrett's esophagus.
This sequence from GER to intestinal metaplasia, dysplasia and adenocarcinoma is now being recognized which translates into a greater understanding and better treatment of the disease.
In contrast, the incidence of squamous cell carcinoma is stable or decreasing.
Symptoms and diagnosis
Dysphagia is the most common presenting symptom. Patients usually present with a history of progressive dysphagia, starting with solid and hard foods (meats and breads) and progressing to soft and liquid foods. Odynophagia, regurgitation and weight loss are also described in advanced cases. Local extension of the tumor invading the tracheobronchial tree or recurrent laryngeal nerve may result in stridor, clogging, coughing, hoarseness, or aspiration pneumonia.
The physical exam is usually normal, but may reveal signs of cachexia as a result of poor nutrition or metastatic disease. Tumors are being diagnosed more frequently in asymptomatic patients with Barrett's esophagus during endoscopic follow-up.
A systemic approach to the diagnosis and staging of esophageal cancer is mandatory. Once the histological diagnosis of esophageal carcinoma was confirmed through endoscopy biopsy, a detailed investigation of the local, regional, and metastatic extent of the disease is necessary. CT scans of the chest and abdomen are useful in the search for metastatic disease. Endoscopic ultrasound may be useful in assessing the depth of tumor invasion and regional lymph node involvement. The accuracy is 80-85% for invasion at depth and 70-75% for nodal status. Accurate pre-treatment staging is important not only for survival analysis but also for clinical decision-making.
Treatment
Treatment can be palliative or curative depending on the stage of the disease and the patient's condition. Curative treatment is mostly applicable in early lesions. If lymph node invasion is limited, moderately advanced tumors may be cured surgically.
The earliest forms of cancer - high-grade dysplasia and carcinoma limited to the mucosa - can be treated with limited esophagectomy with a high expectation of cure.
Therapies targeting endoscopic mucosal ablation for early tumors are still experimental. For more advanced, but still potentially curable, five-year survival rates as high as 41% have been reported. Two recent studies have reported that patients with stage III disease, long-term survival can be achieved in 25-35% of patients following an esophageectomy.
Esophaglutectomy can be performed through the transthoracic or transhiatal route. Morbidity and mortality is less than 10% as a result of improved surgical technique and perioperative care.
The addition of chemo and radiation therapy after surgery (adjuvant therapy) has not been shown to be beneficial. The administration of chemo and preoperative radiotherapy (neo-adjuvancy) is gaining popularity, and may possibly be superior to surgery as the only treatment, but the evidence is not entirely conclusive and the morbidity of surgery may increase with preoperative therapy.
In patients with advanced tumors, the disease is essentially incurable and the focus is on palliation. If the tumor is resectable, the best palliation is usually obtained with surgery. In unresectable tumors or in the presence of distant metastases, survival is much shorter and resective surgery is rarely justified. Dysphagia is well palliated with endoscopic insertion of a stent.
Complications
Mortality from esophaguectomy is 5-10% in specialized units. The results show that esophagetomy is performed more safely in institutions with a high volume of cases. The most common complications are pulmonary (10-50%), cardiac arrhythmias (10%), and anastomotic fistula (5-10%). When anastomosis is performed on the neck, a fistula is rarely responsible for serious morbidity.
However, neck dissection carries the potential risk of temporary or permanent injury to the recurrent laryngeal nerve.
Expected results
The average hospital stay is 10 to 14 days. The average five-year survival after resection is 20-35%. For patients with early tumors limited to the mucosa, five-year survival may exceed 80%. Patients free of lymphatic metastases have a five-year survival of 60%, on the other hand survival drops to 10 -20% in patients with positive nodes. Palliative resection provides relief from dysphagia in 90% of patients.