Barrett's oesophagus
Barrett's oesophagus occurs when the epithelium (the outermost layer of the oesophageal wall) is replaced by another type of epithelium containing intestinal-type cells as a result of ongoing damage from gastroesophageal reflux (which is usually acidic), a condition known as intestinal metaplasia.
There are different types or grades of Barrett's oesophagus, according to the biopsy results and microscopic study. The grades can be:
- Intestinal metaplasia without dysplasia
- Intestinal metaplasia with low-grade dysplasia
- Intestinal metaplasia with high-grade dysplasia
Dysplasia refers to the inherent alterations of a tissue or cell, making it more disorganised and similar to a cancerous cell. Although dysplasia increases cancer risk, it is not considered cancer itself but rather a precancerous lesion. Ultimately, high-grade dysplasia may be considered cancer if there are signs of tissue invasion. As there is a risk of developing oesophageal cancer, it is very important to identify patients with this condition, make an accurate diagnosis, and establish the most precise and effective treatment. That is why our patients have access to the Barrett's Oesophagus Unit, made up of specialists offering the most accurate diagnosis and treatment, as well as the most innovative techniques.
What are the risks for a patient with Barrett's oesophagus?
Barrett’s oesophagus increases the risk of developing oesophageal adenocarcinoma (a specific type of cancer). Although all grades of Barrett’s oesophagus increase the patient’s risk compared to the general population, low- and high-grade dysplasia present the greatest risk.
| DIAGNOSIS | % risk per year | % risk in 4 years |
| Advanced intestinal metaplasia with low-grade dysplasia | 4.3% | 16.1% |
| Advanced intestinal metaplasia with high-grade dysplasia | 0.9% | 3.6% |
| Advanced intestinal metaplasia in oesophageal cancer | 0.5% | 2.0% |
*Data source: Sharma P, Falk GW, Weston AP, et al.
Dysplasia and cancer in a large multicenter cohort of patients with Barrett's esophagus.
Clin Gastroenterol Hepatol 2006; 4:566-572.
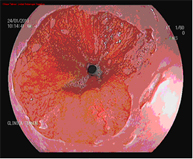
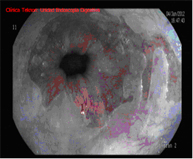
How is diagnosis performed?
Diagnosis is performed using high-resolution magnification endoscopy (image enhancement), employing additional chromoendoscopy techniques conducted by endoscopists specialised in the early diagnosis of premalignant lesions, with targeted biopsies for analysis.


When should Barrett's oesophagus be treated and which technique is indicated in each case?
Barrett's oesophagus should currently only be treated when dysplasia appears and is maintained or confirmed in a follow-up at 3-6 months (depending on the degree of dysplasia), with radiofrequency being the technique of choice if there are no visible lesions. Mucosectomy followed by radiofrequency on the remaining Barrett's oesophagus is the technique of choice if these lesions exist.
Treating Barrett's oesophagus involves controlling acid or gastroesophageal reflux to prevent it from progressing. High-dose treatment with acid production inhibitors is the treatment of choice, with antireflux surgery being considered as an alternative.

Endoscopic Techniques for the Treatment of Barrett's Oesophagus
Endoscopic mucosectomy
Endoscopic mucosal resection involves the endoscopic removal of a section of the mucosa and submucosa (in this case of the oesophagus). It is indicated whenever elevated lesions are observed in Barrett's oesophagus during diagnostic endoscopy.
This diagnostic test is conducted on an outpatient basis, with patients remaining under observation in the day hospital for a few hours.
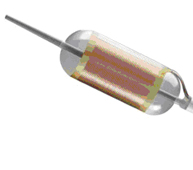
Radiofrequency with HALO system
The HALO radiofrequency ablation system safely and uniformly ablates the oesophageal mucosa to a depth of approximately 1 mm. Ablation is a technique in which tissue is heated until it is no longer viable or alive. HALO technology is a very specific type of ablation where heat energy is applied precisely and in a controlled manner. Clinical trials have demonstrated that Barrett's tissue can be completely eliminated with HALO ablation technology in 98.4% of patients.
Endoscopic follow-up is required, and treatment generally needs to be repeated in one or two sessions.
How should Barrett's oesophagus be monitored?
An initial endoscopy with biopsies should be performed following the Seattle protocol. An endoscopic checkup is recommended after one year if there is no dysplasia but Barrett’s oesophagus is present, simultaneously increasing the dose of the gastric protector or its derivatives and ensuring complete inhibition of acid reflux through pH monitoring.
An endoscopic check is performed every 2-3 years if the second endoscopy still shows no dysplasia and the acid is controlled.
Endoscopic treatment is indicated whenever dysplasia is confirmed in a second checkup.


































